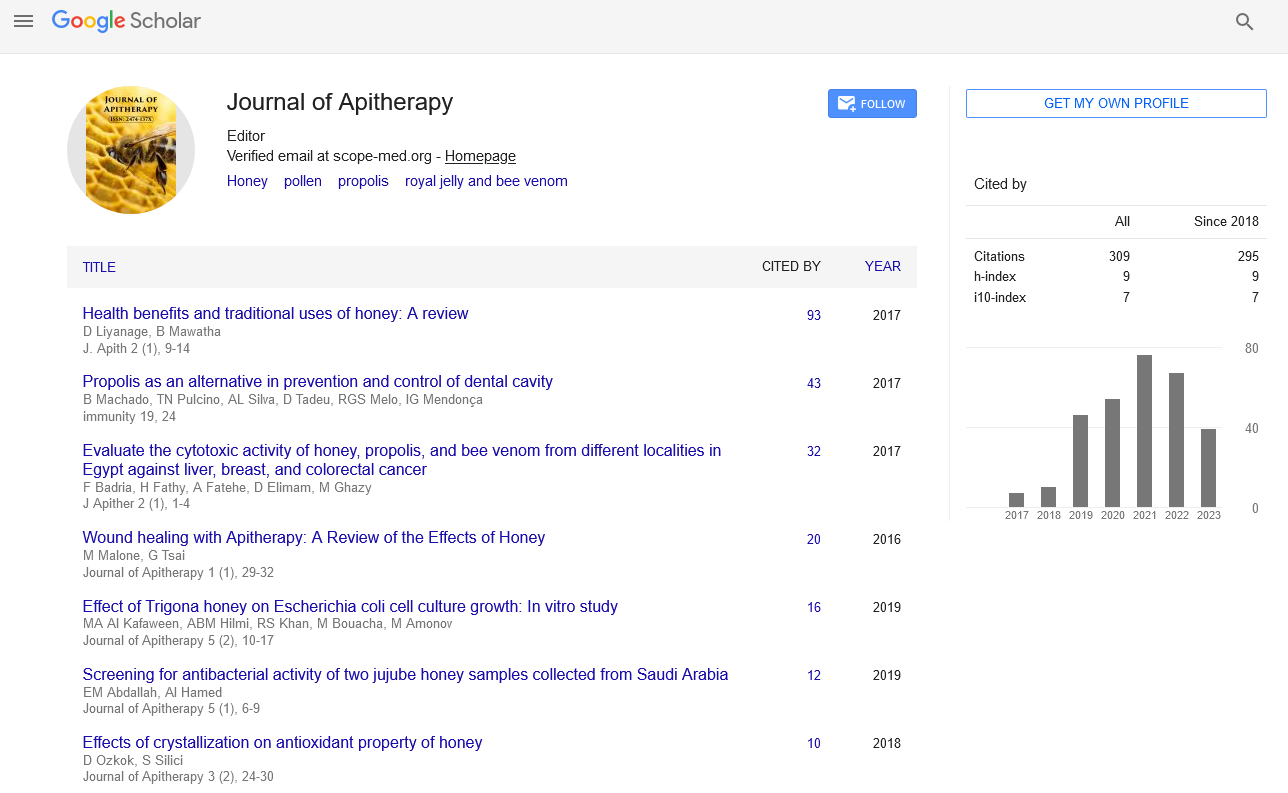
Commentary - Journal of Apitherapy (2022)
A Short Note on Bee Sting Therapy
Stephen Klotz*Stephen Klotz, Department of Medicine, University of Arizona, Tucson, China, Email: duffse05@gmail.com
Received: 15-Mar-2022, Manuscript No. JAPITHERPAY-22-61798; Editor assigned: 17-Mar-2022, Pre QC No. JAPITHERPAY-22- 61798 (PQ); Reviewed: 01-Apr-2022, QC No. JAPITHERPAY-22- 61798; Revised: 08-Apr-2022, Manuscript No. JAPITHERPAY-22- 61798 (R); Published: 15-Apr-2022
Description
Honey bees are distributed all over the world and have an important pollination role in both natural habitats and agriculture. Despite their ability to inject sophisticated venom into their victims as a defence measure, most species are normally docile, and most interactions between humans and bees are unproblematic. Because there are presently no specialised antivenoms against bee venom, therapy for such stings mainly focuses on preventing allergic reactions. Researchers have looked at developing bee antivenoms, but their efforts have been hampered by the primary bee poisons’ poor immunogenicity, which fails to elicit a significant antibody response in immunised animals. Bee stings are the most common human pathologies induced by venomous animals in various nations, outnumbering the fatality rate caused by other venomous species such as snakes, spiders, and scorpions. Anaphylaxis or poisoning is possible symptom following a bee sting. Massive attacks cause the latter, which is a dangerous problem that could endanger the patient’s life. Poisoning causes hemolysis, rhabdomyolysis, and acute renal failure, which, when combined with other systemic failures, can lead to death. Because no antivenoms with established clinical efficacy exist, understanding the physio pathological mechanisms involved in bee mass attacks is critical for health care practitioners. Stings from Hymenoptera can produce local and systemic allergic reactions, as well as life-threatening anaphylaxis. Hymenoptera venom, along with pharmaceutical medications and foods, is one of the most prevalent causes of anaphylaxis in people. Bee stings are a typical occurrence all around the world. After a bee sting, a variety of symptoms have been documented. Reactions at the local level are widespread. Symptoms such as vomiting, diarrhoea, dyspnea, widespread edoema, abrupt renal failure, hypotension, and collapse may develop, which is unusual. In Korea, live bee acupuncture (Bong-Chim) dermatitis is an iatrogenic illness caused by so-called live bee acupuncture therapy, which involves injecting the stinger of a honeybee (Apis cerana) directly into the lesion to treat a variety of disorders. This condition can be classified into three stages: acute, subacute, and chronic. An inflammatory reaction, such as anaphylaxis or urticaria, is the acute stage. In the chronic stage, the leftover stingers may form a foreign body granuloma, similar to a bee stung reaction. Unlike bee stings, however, we see the characteristic histological “flame” figures resulting from eosinophilic stimulation induced by excessive bee venom exposure in the subacute stage. The bee-sting anaphylaxis syndrome is described. Children who have had past adverse reactions to bee stings, particularly those with a history of asthma, are particularly vulnerable. In such circumstances, desensitisation is essential; adrenaline should be stored in the home, and parents should be instructed in how to use it in an emergency. The immunological processes of anaphylaxis caused by bee stings are outlined. Many of the people stung by bees each year have severe systemic reactions, yet the vast majority of these reactions are not life-threatening. There is no evidence that the few people who die as a result of a bee sting come from the same group of people who had a systemic reaction previously. On the other hand, no response at all could be a more alarming sign of a deadly consequence in a subsequent sting. Anaphylaxis isn’t the exclusive cause of death; other factors also play a role. Underlying coronary atherosclerosis appears to be the primary cause of death in this case, as it is in most cases of sudden death. The temperature of the habitat and the location of the sting are two external factors that influence mortality.
Copyright: © 2022 The Authors. This is an open access article under the terms of the Creative Commons Attribution NonCommercial ShareAlike 4.0 (https://creativecommons.org/licenses/by-nc-sa/4.0/). This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.