Research Article - Journal of Apitherapy (2021)
Removal of Basal Cell Carcinoma by Apis Mellifera L Venom
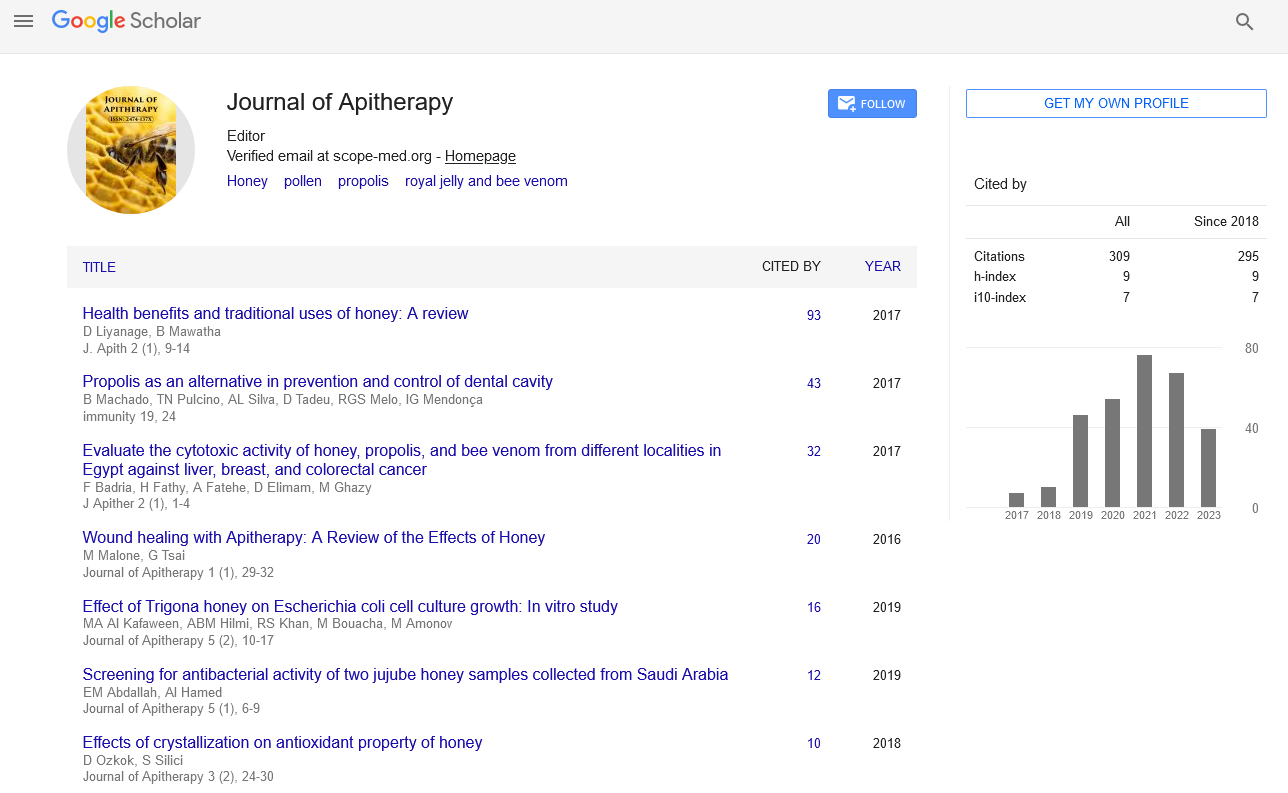
Samia Ahmed Kamal*Samia Ahmed Kamal, Department of Virology, Animal Health Research Institute, Egypt, Email: selkabany@yahoo.com
Published: 01-Mar-2021
Abstract
Background: Honeybee’s venom is potent anticancer drug without exhibiting any side effects. Skin Basal Cell Carcinoma (SBCC) is a common malignancy. It can cause significant local destructions depending on affected site. The diagnosis of SBCC can be suspected from clinical findings and confirmation of diagnosis histopathology. The present SBCC is recurrent and aggressive in the skin of head (upper right, in front of the right ear); the patient was 65 years old in time of first intervention. Materials and Methods: Following the lesions primarily surgically excised, the malignant growths recurrent and visual recognition occurred after 1 year from first operation, then another (the second) surgical removal of SBCC from affected skin with removal of all skin layers near the affected site but another recurrence visually occurs after about 4 months, in the form of malignant growth in the skin of right ear. Dry honeybee’s venom 1 mg was dissolved in 1 ml dist. water as injectable solution. Moreover, ointment contains 2% bee venom was prepared to be used topically inside affected ear as injection is not possible. Results: Before this novel intervention, the desperate patient situation seems very dangerous; as the new growths appear as continuous spread near the removed skin, so that patient’s family decided to apply more noninvasive and non-surgical intervention. The only precaution was testing the patients to assure she is not hypersensitive to honeybees’ venom. The treatment performed by subcutaneous injection of 0.3 ml from prepared Honeybees venom (0.1% conc.) in the skin of affected part of the ear. Subcutaneous infiltration was applied around the lesions of about 0.5 ml as well, topical application of the ointment inside inner part of affected ear. This process repeated daily with cleaning of the ear every time by suitable safe and sterile saline solutions. Management of healing process was enhanced by ascorbic acid solution as topical application on dead cancer cells and to help in exudates debris removal. The complete removal of malignant growths and recovery obtained after 1 month from first bee venom injections. No recurrence of SBCC seen for 3 yrs. Conclusion: Honeybees venom is highly effective and safe anticancer drug that can be used for all patients’ categories of all ages. Regarding the present case invasive surgical intervention was not the good choice from the beginnings, as recurrence and giving chance for spreading following the time lapse between every surgery.
Keywords
Skin basal cell carcinoma; BCC; SBCC; Malignancy of skin; Treatment of cancer; Bee venom; Anti-cancer; Anticancer peptides; Apis mellifera L venom
Introduction
Basal cell carcinoma (BCC), first described by Jacob in 1827 [1]. It is the most common malignant neoplasm of humans. SBCC is highly destructive malignant tumor that spread by invasion to adjacent areas, primarily affecting the skin layers then attacks other tissues (e.g. cartilages, blood vessels). The identification of high risk SBCC types is based on tumor primary origin, invasiveness characteristics and patient clinical factors include demographic information age (old/childhood), immune suppression, organ transplant, prior burn or radiotherapy, and whether this is a primary or recurrent tumor. Tumor-related features include tumor size and location. High risk includes head and neck skin; deeper invasion beyond reticular dermis, ears and neural and lympho-vascular involvement. On rare occasions, a lesion manifests tenderness or pain which can be a clue to perineural infiltration in the aggressive growth varieties. Sensorimotor compromise has been reported particularly in lesions of the pre-auricular and cheek areas [2]. The typical SBCC aggressive growth tumors tend to show more frequent ulceration and large, untended neoplasms can be locally destructive of eyes, ears and nares [3].
The venom of the honeybees’ worker causes certain pain at the site of the sting, moderate swelling and slight reddening. In the act of stinging, the venom sac and attached muscles are torn from the bee, causing its death. The muscles then continue to work the sting deeper into the wound and inject further venom. To prevent this, the sting should be scraped out with a fingernail (not grasped and pulled out, as these forces all remaining venom into the wound) [4]. Some people develop acute allergic reactions to bee stings. An allergic reaction becomes evident in less than an hour and consists of extreme difficulty in breathing, heart irregularity, shock, splotched skin, and speech difficulty. A person showing signs of an allergic reaction should see a medical doctor immediately [5-6]. Bee venom once excreted from bee’s stings is a clear liquid, turns to forms whitish crystals when exposed to air. Bee venom is a mixture of histamine, pheromones, enzymes, peptides, amino acids and other acids, with over 100 components in total. The main enzymes present are phospholipase A, hyaluronidase, and lecithinase; while the main peptides are mellitin, apamin and peptide 401 (a powerful anti-inflammatory agent). Mellitin, a cationic peptide of 26 amino acid length, makes up 50% of the dry weight of bee venom, and acts as anticoagulants. It also lowers blood pressure, causes histamine release. Both mellitin and apamin cause the body to release cortisol, a natural steroid, while peptide 401 is a powerful anti-inflammatory agent. The main amino acids in bee venom are cysteine and methionine, both of which contain sulphur. Sulphur is important in inducing cortisol release from the adrenal glands. Histamine makes up 0.9% of venom, and causes itching and pain at the site of the sting. The acids present, which include formic, hydrochloric and orthophosphoric acids, are now believed to be much less important in causing pain than was previously thought. Honeybee Venom (HBV) has been recognized as anti-cancer drug in vitro and in vivo (stings of honeybees on the affected area or the extracted bee venom by intramuscular injection). The venom stimulates the release of cortisol, and so is effective in the treatment of rheumatic disorders such as Multiple Sclerosis, rheumatoid arthritis and gout. Mellitin is believed to be the main active agent. Bee venom therapy is one aspect of apitherapy (use of bee products for curing disease). Mellitin is also being investigated as an anti-cancer agent. By modifying the mellitin molecule to prevent allergic reaction, and attaching a cancer-specific antibody (this combination of toxin and antibody is called an immunotoxin), researchers hope to produce a ‘magic bullet’ treatment- so called because it would only destroy cancer cells (unlike conventional chemotherapy agents, which destroy all types of cell, causing unpleasant side effects such as vomiting and hair loss) [6-29].
Material and Methods
Following the lesions primarily surgically excised, the malignant growths recurrent and visual recognition occurred after 1 year from first operation, then another (the second) surgical removal of SBCC from affected skin with removal of all skin layers near the affected site but another recurrence visually occurs after about 4 months, in the form of malignant growth in the skin of right ear. Dry honeybee’s venom 1 mg was dissolved in 1 ml dist. water as injectable solution. Moreover, ointment contains 2% bee venom was prepared to be used topically inside affected ear as injection is not possible.
Materials
b-Extraction of honeybee venom: The electrical shock method has been used to stimulate the bees to sting. The collector frame placed at the entrance of the hive and connected to a device which supplies electrical impulses, when bees receive a mild electric shock; they sting the surface of the collector sheet as they see this to be the source of danger. However, Honeybees didn’t die after stinging the plate. The deposited venom between the glass and the protective material was dried then later scrapped off by a razor blade and collected in a dark bottle (Figure 1).
c-Ascorbic acid (Vitamin C): It was white crystalline powder, soluble in water. Concentrated solution was prepared in phosphate buffer solution (PBS).
d. Clove oil: Bee venom diluted solution 0.1% was added to the oil in a ratio of 1/10 (bee venom/clove oil).
Methods
Bee venom subcutaneous injection of superficial lymph nodes: The process of using bee venom should be suitable and unique for every single case. Management of the application process should be mindfully and logic. Injection in the axillary lymph nodes by safer doses daily in cancer patient is of very priority. So that, the present patient receive daily dose of 0.3 ml bee venom (safe concentration) in each axillary lymph nodes as subcutaneous injection (However, in case of swollen lymph nodes anywhere of patient’s body should also receive bee venom as S/C injections). In the present case, application of bee venom was performed locally on the site of carcinoma (skin around the right ear) and the axillary lymph nodes were the targets of the drug.
The stages of treatment: The signs of relief were after first injection, as the irritations and annoyance inside the ear shows instant relief and completely disappeared after only one week of bee venom therapy. The affected skin which was showing thickening and color changes become gradually smaller in size, with disappearance of the malignant growths picture from the affected area. Pus and exudates were accumulated after application of the topical ointment inside the ear, which removed and cleaned before each injection. The ear returned to normal status with comments of patient that she is hearing normally from the affected ear, feel signs of relief and health. These effects were seen after 10 days only from first bee venom application. The tumor area became smaller and smaller with color changes disappeared gradually (Figures 2-8).
For help in slowing local spreading of BCC, and avoiding accumulation of exudates inside the affected ear, the instructions were given for patient to sleep on the right side of body and putting the affected ear down during sleeping against the gravity. Complete rest is recommended. It is noted that after the injection of bee venom, the cancerous growths died and the exudates of dead cells were leaking from the affected skin. The strong effect of bee venom on these cancerous was specifically rapid and without any side effects.
Addition of ascorbic acid (Vitamin C): A concentrated solution of vitamin C dissolved in saline solution was prepared for topical use as a dressing over the affected skin. The use of vitamin C helped to get rid of pus and dead tissue in the affected area. The growth of cancer within the skin of the ear made us have to focus on the injection of bee venom under the skin around the ear and not inside the ear.
Clove oil mixed with bee venom for topical application: Clove oil mixed with bee venom, the drug prepared in order to deliver the medicine to the diseased ear; we poured the mixture into the ear and left it for up to 8 hours in order to give the opportunity to absorb the medicine. Clove oil is a volatile oil that contains antimicrobial agents, palliatives and pain relievers. The ulcerative lesions clean up after using this mixture. It applied alternatively as dressing over the malignant growths. The mixture showed good results as the injury appeared to be clean from the dead tissue and from the pus, as it accelerated the elimination of parts of the cancerous growth by turning it into exudates of pus like material, which washed out by thorough cleaning. Application of this method was performed until disappearance of cancer and completes healing.
Results
Honeybee’s venom is potent anticancer drug without exhibiting any side effects. Skin Basal Cell Carcinoma (SBCC) is a common malignancy. SBCC has almost no reports of tendency for metastasis. It can cause significant local destructions depending on affected site. The diagnosis of SBCC can be suspected from clinical findings and confirmation of diagnosis histopathology. The present SBCC is recurrent and aggressive in the skin of head (upper right, in front of the right ear); the patient was 65 years old in time of first intervention.
Following the lesions primarily surgically excised, the malignant growths recurrent and visual recognition occurred after 1 year from first operation, then another (the second) surgical removal of SBCC from affected skin with removal of all skin layers near the affected site but another recurrence visually occurs after about 4 months, in the form of malignant growth in the skin of right ear. Dry honeybee’s venom 1 mg was dissolved in 1 ml dist. water as injectable solution. Moreover, ointment contains 2% bee venom was prepared to be used topically inside affected ear as injection is not possible.
Basal cell carcinoma spreading behavior
The lesions extended laterally from previous sites; showings fingers channels through affected tissue, which appears blackish brown in color, under the grafted skin, it extends fingers in the deep tissue. Bee venom destruct these fingers with highly selective manner, as the drug only destroy the neoplastic growths, leaving healthy tissue with its normal blood capillaries. The gross picture of the lesions different in the course of treatment, the unapparent neoplastic growths was observed after removal of the destructed lesions, exhibiting the pathway of tumor cells spreading. Local injection was highly recommended, as it destroys abnormal cells and pointed the sites of the unapparent subcutaneous neoplastic lesions (Figures 3-5).
Before this novel intervention, the desperate patient situation seems very dangerous; as the new growths appear as continuous spread near the removed skin, so that patient’s family decided to apply more noninvasive and non-surgical intervention. The only precaution was testing the patients to assure she is not hypersensitive to honeybees’ venom. The treatment performed by subcutaneous injection of 0.3 ml from prepared Honeybees venom (0.1% conc.) in the skin of affected part of the ear. Subcutaneous infiltration was applied around the lesions of about 0.5 ml as well, topical application of the ointment inside inner part of affected ear. This process repeated daily with cleaning of the ear every time by suitable safe and sterile saline solutions. Management of healing process was enhanced by ascorbic acid solution as topical application on dead cancer cells and to help in exudates debris removal. The complete removal of malignant growths and recovery obtained after 1 month from first bee venom injections. No recurrence of SBCC seen for 3 yrs. (Figures 6-8)
Discussion
Skin Basal Cell Carcinoma (SBCC) is a common malignancy affecting most probably populations with light skin. SBCC can cause significant local destructions depending on affected site. Biological transformation of BCC tends to occur at the base and edges of the growing neoplasm. The diagnosis of BCC can be suspected from clinical findings and confirmation of diagnosis requires histopathology of biopsy [1-3].
Malignant tumor of basal cell carcinoma of hairy skin of the head and the ear, the anticancer effects of Apis mellifera L’s venom (Honeybees) drug as injectable solutions (0.1% the safe dose), have the potency to treat these conditions and preventing the spread of cancer. Bee venom is potent drug, with zero side effects in cases not hypersensitive against it. It cures the affected skin in very short time, without disfiguration of the patient body parts. Surgery was wrong choice in this case, giving more time for tumor cells to spread to the adjacent areas, leaving patients suffering another surgical intervention with permanent disfiguration of skin. Very small percentages of human have showed skin allergy from bee venom. However, Bee venom is safe drug when used in the recommended doses. Doses of bee venom which consider safe depends upon age, health conditions, type of illness, degree of affections, severity of illness, however in malignancy it is of special regime for every single case, depending on the practitioner experience and knowledge which should be of higher level [15-29].
Bee venom (Apis mellifera L) is safe and effective anticancer drug. As described by Cassier et al., (1994) study the contribution of the sting sheaths of the worker to the defensive behavior of a bee colony. The structure of the proximal part of the sting sheath integument has all the characteristics of a primitive exocrine gland: porous cuticle with enlarged pore canals and epicuticular pores, and hypertrophied epithelial cells secreting an electron dense material. The non-volatile part of the secretory product embedded the setae of the sheaths. Individual recipient guards in the laboratory and as a group at hive entrances in a bee yard displayed defense behavior only when stimulated with either sting sheaths or with setaceous membrane, but not with any other gland or organ. Enhanced defensive reaction of guards has been observed when a venom gland or Koschewnikow’s glands are added to either sting sheaths or to setaceous membrane. We demonstrate for the first time that the sting sheaths have the structure of an exocrine gland and that their secretions induce defensive behavior in guards [4]. In agreement with: Moreau, (2012) who mentioned that many hymenopteran species, whatever their life style, have also evolved venom with properties which enable it to regulate microbial infections. Stinging Hymenoptera seems to constitute an under-exploited ecological niche for agents of vector-borne disease. Few parasitic or mutualistic microorganisms have been reported to be hosted by venom-producing organs or to be transmitted to stung animals. This may result from the presence of potent antimicrobial molecules in venoms, histological features of venom apparatuses and selective effects of venoms on immune defenses of targeted organisms [5]. In accordance with: Islam et al., (2017) have mentioned that Melittin (MEL), a major peptide component of bee venom, is an attractive candidate for cancer therapy. This agent has shown a variety of anti-cancer effects in preclinical cell culture and animal model systems [6].
In accordance with: Xinjing Wang et al., (2017) have investigated the anti-cancer activity of melittin and its regulated mechanism(s) in the PDAC models. Melittin was found to suppress tumor growth by promoting cell apoptosis and cell-cycle arrest. Their study has indicated that melittin is capable of suppressing tumor growth and promoting gemcitabine sensitivity in PDAC by down regulating cholesterol pathway [7]. In accordance with: Miran Jo et al., (2011) have investigated whether bee venom and melittin, a major component of bee venom, inhibit cell growth through enhancement of death receptor expressions in the human ovarian cancer cells, SKOV3 and PA-1. Bee venom (1–5 μg/ml) and melittin (0.5–2 μg/ml) inhibited the growth of SKOV3 and PA-1 ovarian cancer cells by the induction of apoptotic cell death in a dose dependent manner. Consistent with apoptotic cell death, expression of death receptor (DR) 3 and DR6 was increased in both cancer cells, but expression of DR4 was increased only in PA-1 cells. They results suggest that bee venom and melittin induce apoptotic cell death in ovarian cancer cells through enhancement of DR3, DR4, and DR6 expression and inhibition of STAT3 pathway [8]. In accordance with: Jeong-Eun Huh et al., (2009) have mentioned that honeybees’s venom significantly inhibited the viability of Lewis lung carcinoma (LLC) cells but did not affect peripheral blood mononuclear lymphocytes (PBML) cells. BV also inhibited vascular endothelial growth factor (VEGF)-induced proliferation, migration and capillary-like tube formation of human umbilical vein endothelial cells (HUVECs). The western blotting analysis showed that BV inhibited AKT and MAPK phosphorylation in LLC cells and HUVECs and down regulated expression of VEGF and VEGFR-2 of LLC cells and HUVECs. They discover that Bee Venom effectively disrupted VEGF-induced neovascularization in Matrigel plugs in their in vivo angiogenesis assay. When given subcutaneously, Bee Venom was significantly suppressed tumor angiogenesis through inhibition of VEGF and VEGFR-2 in LLC model. Mice bearing subcutaneous LLC tumors were treated with 1 μg/ml or 10 μg/ml of Bee Venom, showing reductions ranging between 49% and 62% in primary tumor volume and reduction of spontaneous pulmonary metastasis occurrences. Furthermore, BV treatment in the spontaneous lung metastases model after primary tumor excision prolonged their median survival time from 27 to 58 days. These results suggest that the tumor-specific anti-angiogenic activity of Bee Venom takes effect during different stages of tumor progression by blocking the tyrosine phosphorylation of VEGFR-2, and validate the application of BV in lung cancer treatment [9]. In accordance with: Son et al., (2007) have mentioned BV contains a variety of peptides, including melittin, apamin, adolapin, the mast-cell-degranulating (MCD) peptide, enzymes (i.e., phospholipase (PL) A (2), biologically active amines (i.e., histamine and epinephrine), and non-peptide components which have a variety of pharmaceutical properties [10]. In accordance with: Oršolić, (2012) who mentioned that honeybee’s venom has been used in the treatment of some immune-related diseases, as well as in treatment of tumors. Several cancer cells, including renal, lung, liver, prostate, bladder, and mammary cancer cells as well as leukemia cells, can be targets of bee venom peptides such as melittin and phospholipase A2. The cell cytotoxic effects through the activation of PLA2 by melittin have been suggested to be the critical mechanism for the anti-cancer activity of BV. The induction of apoptotic cell death through several cancer cell death mechanisms, including the activation of caspase and matrix metalloproteinases, is important for the melittin-induced anti-cancer effects [11].
However, the antimicrobial effects of bee venom are overwhelming. Socarras et al., (2017) have mentioned that Lyme disease is a tick-borne, multi-systemic disease, caused by the bacterium Borrelia burgdorferi. Though antibiotics are used as a primary treatment, relapse often occurs after the discontinuation of antimicrobial agents. The reason for relapse remains unknown, however previous studies suggest the possible presence of antibiotic resistant Borrelia round bodies, persisters and attached biofilm forms. Thus, there is an urgent need to find antimicrobial agents suitable to eliminate all known forms of B. burgdorferi. In this study, natural antimicrobial agents such as Apis mellifera venom and a known component, melittin, were tested using SYBR Green I/PI, direct cell counting, biofilm assays combined with LIVE/DEAD and atomic force microscopy methods. The obtained results were compared to standalone and combinations of antibiotics such as Doxycycline, Cefoperazone, Daptomycin, which were recently found to be effective against Borrelia persisters. Our findings showed that both bee venom and melittin had significant effects on all the tested forms of B. burgdorferi. In contrast, the control antibiotics when used individually or even in combinations had limited effects on the attached biofilm form. These findings strongly suggest that whole bee venom or melittin could be effective antimicrobial agents for B. burgdorferi; however, further research is necessary to evaluate their effectiveness in vivo, as well as their safe and effective delivery method for their therapeutic use [12]. In accordance with: Park et al., (2011) have mentioned that Bee venom (1-10 μg/ml) and melittin (0.5-2.5 μg/ml) inhibited cancer cell growth through induction of apoptotic cell death in LNCaP, DU145, and PC-3 human prostate cancer cells (in vitro study). These effects were mediated by the suppression of constitutively activated NF-κB. Bee venom and melittin decreased anti-apoptotic proteins but induced pro-apoptotic proteins. However, pan caspase inhibitor abolished bee venom and melittin-induced apoptotic cell death and NF-κB inactivation. Bee venom (3-6 mg/kg) administration to nude mice implanted with PC-3 cells resulted in inhibition of tumor growth and activity of NF-κB accompanied with apoptotic cell death (in vivo study). Therefore, these results indicated that bee venom and melittin could inhibit prostate cancer in vitro and in vivo, and these effects may be related to NF-κB/ caspase signal mediated induction of apoptotic cell death [13].
In accordance with: Zheng et al., (2015) have mentioned that Bee venom (BV) has been used as a traditional medicine to treat arthritis, rheumatism, back pain, cancerous tumors, and skin diseases. They found that BV inhibited growth of colon cancer cells through induction of apoptosis, also found that the expression of death receptor (DR) 4, DR5, p53, p21, Bax, cleaved caspase-3, cleaved caspase-8, and cleaved caspase-9 was increased by BV treatment in a dose dependent manner (0-5 μg/ml). Consistent with cancer cell growth inhibition, the DNA binding activity of nuclear factor kappa B (NF-κB) was also inhibited by BV treatment. Besides, they found that BV blocked NF-κB activation by directly binding to NF-κB p50 subunit. Moreover, combination treatment with BV and p50 siRNA or NF-κB inhibitor augmented BV-induced cell growth inhibition. However, p50 mutant plasmid (C62S) transfection partially abolished BV-induced cell growth inhibition. BV significantly suppressed tumor growth in vivo. Therefore, these results suggested that BV could inhibit colon cancer cell growth, and these anti-proliferative effects may be related to the induction of apoptosis by activation of DR4 and DR5 and inhibition of NF-κB [14].
Conclusion
Honeybee’s venom is highly effective and safe anticancer drug that can be used for all patients’ categories of all ages. Regarding the present case invasive surgical intervention was not the good choice from the beginnings, as recurrence and spreading follows. The rapid response and the healing effects of bee venom have certain positive psychological effects on family and the patient, after they were very sorry and worried about the progress and spread of cancer, they became more hopeful and happy after only few days from treatment by bee venom. This novel method has been protecting the patient from the severe painful surgical intervention. It is more effective, safe and more successful in removing BCC.
Authors’ Contribution
Prof. Dr. Samia Ahmed Kamal; PhD (Pathology, Cairo Univ.) is the author of this research; who funded, conceived and designed the experiments; performed the experiments; reviewed and edited the manuscript and has contributed to the interpretation and discussion of the results, and approved the final version of the manuscript for publication.\
Availability of Data and Materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
The patient and her family seek bee venom treatment after failure of multiple surgery and recurrence attacking vital organs (the ear). Fearing from spread to the brain, and destroying the ear, with life threatening conditions, they agree and seek this treatment.
Competing Interests
The authors declare that they have no competing interests.
References
- Jacob A. Observations respecting an ulcer of peculiar character, which attacks the eyelids and other parts of the face. Dublin Hospital Rep Commun Med Surg 1827; 4: 232-239.
- McKenzie CA, Chen AC, Choy B, Fernández-Peñas P, Damian DL, Scolyer RA. Classification of high risk basal cell carcinoma subtypes: experience of the ONTRAC study with proposed definitions and guidelines for pathological reporting. Pathology 48:395-397.
- Niazi ZBM, Lamberty BGH. Perineural infiltration in basal cell carcinomas. British Journal of Plastic Surgery 46; 156-157.
- Cassier P, Tel-Zur D, Lensky Y. The sting sheaths of honey bee workers (Apis mellifera L.): Structure and alarm pheromone secretion. J Insect Physiology 40; 23-32.
- McKenna W. killer bees: what the allergist should know. Pediatr. Asthma allergy and immunol 1993; 6:275-285.
- Moreau SJM. It stings a bit but it cleans well: Venoms of Hymenoptera and their antimicrobial potential. J Insect Physiology 2013; 59:186-204.
- Islam R, Imtiaz AS, Mohamad R, Hasan M. Melittin, a major peptide component of bee venom, and its conjugates in cancer therapy. Cancer Letters 2017; 402:16-31.
- Xinjing Wang. Melittin inhibits tumor growth and decreases resistance to gemcitabine by downregulating cholesterol pathway gene CLU in pancreatic ductal adenocarcinoma. Cancer Letters 2017; 399:1-9.
- Miran Jo. Anti-cancer effect of bee venom toxin and melittin in ovarian cancer cells through induction of death receptors and inhibition of JAK2/STAT3 pathway. Toxicology and Applied Pharmacology 2011; 258:72-81.
- Jeong-Eun Huh. Bee venom inhibits tumor angiogenesis and metastasis by inhibiting tyrosine phosphorylation of VEGFR-2 in LLC-tumor-bearing mice. Cancer Letters 2009; 292:98-110.
- Son DJ, Lee JW, Lee YH, Song HS, Lee CK, Hong JT. Therapeutic application of anti-arthritis, pain-releasing, and anti-cancer effects of bee venom and its constituent compounds. Pharmacol Ther 2007; 115(2):246-70.
- Oršolic N. Bee venom in cancer therapy. Cancer Metastasis Rev 2012; 31:173-94.
- Socarras KM, Theophilus PAS, Torres JP, Gupta K, Sapi E. Antimicrobial activity of bee venom and melittin against Borrelia burgdorferi. Antibiotics (Basel) 2017; 6(4). pii: E31.
- Park MH, Choi MS, Kwak DH, Oh KW, Yoon DY, Han SB, et al. Anti-cancer effect of bee venom in prostate cancer cells through activation of caspase pathway via inactivation of NF-?B. Prostate 2011; 71(8):801-12.
- Zheng J, Lee HL, Ham YW, Song HS, Song MJ, Hong JT. Anti-cancer effect of bee venom on colon cancer cell growth by activation of death receptors and inhibition of nuclear factor kappa B. Oncotarget 2015; 6(42):44437-51.
- Sumikura H, Anderson OK, Drewes AW, Arendt-Nelsen LA. A comparision of hyperalgesia and neurogenic inflammation induced by melittin and capsaicin in humans. Neurosci Lett 2003; 337:147-150.
- Nam KW, Je KH, Lee JH, Kang SK, Mar W. Inhibition of COX-2 activity and pro-inflammatory cytokines (TNF-alpha and IL-1beta) production by water soluble sub-fractionated parts from honeybee (Apis melifera) venom. Archiv Pharmacol Res 2003; 26: 383-388.
- Park HJ, Lee SH, Son DJ, Oh KW, Kim KH, Song S, et al. Antiarthritic effect of bee venom: Inhibition of inflammation mediator generation by suppression of NF-kB through interaction with the p50 subunit. Arthritis Rheumatism 2004; 50: 3504-3515
- Jang HS, Kim SK, Han JB, Ahn HJ, Bae H, Min BI. Effects of bee venom on the pro-inflammatory responses in RAW264.7 macrophage cell line. J Ethnopharmacol 2005; 99: 157-160.
- Amin MA, Abdel-Raheem IT, Madkor HR. Wound healing and anti-inflammatory activities of bee venom-chitosan blend films. J Drug Delivery Sci Technol 2008; 18:424-430.
- Yoon SY, Kwon YB, Kim HW, Roh DH, Seo HS, Han HJ, et al. Bee venom injection produces a peripheral anti-inflammatory effect by activation of a nitric oxide-dependent spinocoeruleus pathway. Neurosci Lett 2008; 430: 163-168.
- Habermann E. Chemistry, pharmacology and toxicology of bee, wasp and hornet venoms. In: Bucherl W, Buckley EE Eds., Venomous Animals and Their Toxins: Venomous Invertebrates 1971; 3:61â??93.
- Banks BEC, Shipolini RA. Chemistry and pharmacology of honeybee venom. In: Piek T Ed., Venoms of the Hymenoptera. Academic Press, London 1986; 329â??416.
- Lee JH, Kwon YB, Han HJ, Mar WC, Lee H, Yang IS, et al. Bee venom Pre-treatment has both an anti-nociceptive and anti-inflammatory effect on carrageenan induced inflammation. J Vet Med Sci 2001; 63:251-259.
- Pham Duy Lam, Prabhat Kumar Mandal, Seung Yang Hak, Seong-Gu Hwang. Study of the molecular mechanism of anti-inflammatory activity of bee venom in lipopolysaccharide stimulated raw 264.7 Macrophages. Trop J Pharm Res 2010; 9 (1): 19.
- Chen YN, Li KC, Li GW, Shang D, Liu NZ, Lu M, et al. Pain hypersensitivity in mammals, and among the five identified reverse-phase high pressure liquid chromatography. Neurosci 2005; 138: 631-640.
- Schumacher MJ. Significance of Africanized bees for public health. Arch Med Intern 1993; 155:2038-2043.
- Guillaume C, Calzada C, Lagarde M, Schrével J, Deregnaucourt C. Interplay between lipoproteins and bee venom phospholipase A2 in relation to their anti-plasmodium toxicity. J Lipid Res 2006; 47:1493 - 1506.
- Fenard D, Lambeau G, Maurin T, Lefebvre JC, Doglio A. A peptide derived from bee venom-secreted phospholipase A2 inhibits replication of T-cell tropic HIV- 1 strains via interaction with the CXCR4 chemokine receptor. Mol Pharmacol 2001;60:341-347.